Characterization and In Vitro Evaluation of Silver Nanoparticles Synthesized from Ficus deltoidea for Wound Closure and Skin Regeneration
Main Article Content
Abstract
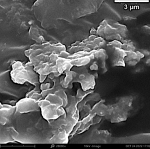
Ficus deltoidea (F. deltoidea), a medicinal plant known for its antioxidant and regenerative properties, has shown therapeutic potential in wound care. However, the potential of silver nanoparticles synthesized from F. deltoidea (Fd-AgNPs) for enhancing wound healing remains underexplored. This study evaluated topical ointments containing green-synthesized Fd-AgNPs at 10%, 20%, and 30% concentrations. The Fd-AgNPs were produced from F. deltoidea ethanolic leaf extract and characterized via UV‒Vis spectrophotometry, scanning electron microscopy (SEM), Fourier transform infrared (FTIR) spectroscopy, and X-ray diffraction (XRD) analyses. Mice with full-thickness skin wounds received daily ointment treatments for 15 days. Wound healing progression was assessed through closure rates, histology, and biochemical markers, including protein content, hydroxyproline levels, total DNA, and fibroblast count. Among the treatments, 10% Fd-AgNP (T4) ointment resulted in complete wound closure by day 12 but yielded the lowest number of fibroblasts (1.58 ± 0.00) and substantial hydroxyproline content (3146.50 ± 79.54 µg/mL). Moreover, T5 (20%) presented higher protein (961.81 ± 90.67 µg/mL) and DNA levels (4.10 ± 0.15 µg/mL) than the other groups did, whereas T6 (30%) presented intermediate values for most markers (protein and DNA) between T4 and T5. Histological analysis confirmed improved tissue regeneration in mice treated with any concentration of Fd-AgNP topical ointment. These findings confirmed that Fd-AgNPs topical ointment enhances wound regeneration by promoting fibroblast proliferation and extracellular matrix synthesis. The study concluded that 20% Fd-AgNP ointment may offer an optimal equilibrium between healing velocity and quality, rendering it the most promising formulation for attaining both rapid and structurally robust wound healing.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Cite
References
1. Abdulrahman MD. Crude extract of Ficus deltoidea Jack (FD) as a natural biological therapy. Explor target anti-tumor ther. 2023; 4(1):57–88. DOI: https://doi.org/10.37349/etat.2023.00123
2. Raihandhany R, Zen TV. Exploring the less prominent relatives of Ficus benjamina L. in Indonesia A review on the botanical, ethnobotanical, and future perspectives of Ficus deltoidea Jack. and Ficus septica Burm. f. Genbinesia J Biol. 2022; 1(2):76-89.
3. Abrahim NN, Abdul-Rahman PS, Aminudin N. The antioxidant activities, cytotoxic properties, and identification of water-soluble compounds of Ficus deltoidea leaves. PeerJ. 2018; 6:1-20. DOI: https://doi.org/10.7717/peerj.5694
4. Ashraf K, Haque MR, Amir M, Ahmad N, Ahmad W, Sultan S, Shah SAA, Alafeefy AM, Mujeeb M, Shafie MFB. An Overview of Phytochemical and Biological Activities: Ficus deltoidea: Jack and Other: Ficus: spp. J Pharm Bioallied Sci. 2021; 13(1):11-25. DOI: https://doi.org/10.4103/jpbs.JPBS_232_19
5. Aryani R, Nugroho RA, Manurung H, Mardayanti R, Prahastika W, Karo APB. Ficus deltoidea leaves methanol extract promote wound healing activity in mice. EurAsian J BioSci. 2020; 14(1):85-91.
6. Lakkim V, Reddy MC, Lekkala VV, Lebaka VR, Korivi M, Lomada D. Antioxidant efficacy of green-synthesized silver nanoparticles promotes wound healing in mice. Pharmaceutics. 2023; 15(5):1517. DOI: https://doi.org/10.3390/pharmaceutics15051517
7. Mamun AA, Shao C, Geng P, Wang S, Xiao J. Recent advances in molecular mechanisms of skin wound healing and its treatments. Front Immunol. 2024; 15(1):1-29. DOI: https://doi.org/10.3389/fimmu.2024.1395479
8. Venkatesan K, Sivadasan D, Abderrahmen Al Weslati M, Gayasuddin Mouid M, Goyal M, Bansal M, Salama ME-DM, Azizullah Ghori S, Ahmad F. Protective Effects of Frankincense Oil on Wound Healing: Downregulating Caspase-3 Expression to Facilitate the Transition from the Inflammatory to Proliferative Phase. Pharmaceuticals. 2025; 18(3):407. DOI: https://doi.org/10.3390/ph18030407
9. Cioce A, Cavani A, Cattani C, Scopelliti F. Role of the skin immune system in wound healing. Cells. 2024; 13(7):624. DOI: https://doi.org/10.3390/cells13070624
10. Suhag D. Skin and Wound Healing Biomaterials. Handbook of Biomaterials for Medical Applications, Volume 2: Applications: Springer; 2024. p. 281-320. DOI: https://doi.org/10.1007/978-981-97-5906-4_9
11. Uberoi A, McCready-Vangi A, Grice EA. The wound microbiota: microbial mechanisms of impaired wound healing and infection. Nat Rev Microbiol. 2024; 22(8):507-521. DOI: https://doi.org/10.1038/s41579-024-01035-z
12. Kumar P, Hasan F, Kumar V, Chawla R, Goyal SK. Diabetic Wound Healing: Navigating Physiology, Advancements and Research Frontiers. J Diabetes Res. 2024; 6(2):1-11. DOI: https://doi.org/10.47363/JDRR/2024(6)181
13. Pramasari N, Anjani AG, Muslikh FA, Lestari TP, Shoviantari F, Septyaningrum SD, Melati IS, Randy GY. Green Synthesis, Optimization and Characterization of Carrot Extract Silver Nanoparticles. Trop J Pharm Res. 2024; 8(12):1-5. DOI: https://doi.org/10.26538/tjnpr/v8i12.35
14. Alavi SE, Alavi SZ, Nisa MU, Koohi M, Raza A, Ebrahimi Shahmabadi H. Revolutionizing wound healing: exploring scarless solutions through drug delivery innovations. Mol Pharm. 2024; 21(3):1056-1076. DOI: https://doi.org/10.1021/acs.molpharmaceut.3c01072
15. Banerjee D, Vydiam K, Vangala V, Mukherjee S. Advancement of Nanomaterials-and Biomaterials-Based Technologies for Wound Healing and Tissue Regenerative Applications. ACS Appl Bio Mater. 2025; 8(3):1877–1899. DOI: https://doi.org/10.1021/acsabm.5c00075
16. Ullah A, Ullah M, Lee G-J, Lim SI. A review of recent advances in nanotechnology for the delivery of therapeutics in wound healing. J Pharm Investig. 2025; 55(1):33-54. DOI: https://doi.org/10.1007/s40005-024-00692-9
17. Jangid H, Singh S, Kashyap P, Singh A, Kumar G. Advancing biomedical applications: An in-depth analysis of silver nanoparticles in antimicrobial, anticancer, and wound healing roles. Front Pharmacol. 2024; 15(1):1-26. DOI: https://doi.org/10.3389/fphar.2024.1438227
18. Nqakala ZB, Sibuyi NR, Fadaka AO, Meyer M, Onani MO, Madiehe AM. Advances in nanotechnology towards development of silver nanoparticle-based wound-healing agents. Int J Mol Sci. 2021; 22(20):1-26. DOI: https://doi.org/10.3390/ijms222011272
19. Naganthran A, Verasoundarapandian G, Khalid FE, Masarudin MJ, Zulkharnain A, Nawawi NM, Karim M, Che Abdullah CA, Ahmad SA. Synthesis, characterization and biomedical application of silver nanoparticles. Materials. 2022; 15(2):427. DOI: https://doi.org/10.3390/ma15020427
20. Ranjbar S, Bakhtiari A, Khosravi N, Ashkavandi SJ, Azamian F, Alijaniha M, Karbalaee M. Silver nanoparticles: Biomedical applications and future perspectives. JCC. 2024; 6(20):1-13. DOI: https://doi.org/10.61186/jcc.6.3.2
21. Ren Y, Zhang Y, Li X. Application of AgNPs in biomedicine: An overview and current trends. Nanotechnol Rev. 2024; 13(1):1-17. DOI: https://doi.org/10.1515/ntrev-2024-0030
22. More PR, Pandit S, Filippis AD, Franci G, Mijakovic I, Galdiero M. Silver nanoparticles: bactericidal and mechanistic approach against drug resistant pathogens. Microorganisms. 2023; 11(2):369-396. DOI: https://doi.org/10.3390/microorganisms11020369
23. Tripathi N, Goshisht MK. Recent advances and mechanistic insights into antibacterial activity, antibiofilm activity, and cytotoxicity of silver nanoparticles. ACS Appl Bio Mater. 2022; 5(4):1391-1463. DOI: https://doi.org/10.1021/acsabm.2c00014
24. Fu W, Sun S, Cheng Y, Ma J, Hu Y, Yang Z, Yao H, Zhang Z. Opportunities and challenges of nanomaterials in wound healing: Advances, mechanisms, and perspectives. Chem Eng J. 2024:153640. DOI: https://doi.org/10.1016/j.cej.2024.153640
25. Nandhini J, Karthikeyan E, Rani EE, Karthikha V, Sanjana DS, Jeevitha H, Rajeshkumar S, Venugopal V, Priyadharshan A. Advancing engineered approaches for sustainable wound regeneration and repair: Harnessing the potential of green synthesized silver nanoparticles. Eng Regen. 2024; 5(3):306-325. DOI: https://doi.org/10.1016/j.engreg.2024.06.004
26. Sati A, Ranade TN, Mali SN, Ahmad Yasin HK, Pratap A. Silver Nanoparticles (AgNPs): Comprehensive Insights into Bio/Synthesis, Key Influencing Factors, Multifaceted Applications, and Toxicity─ A 2024 Update. ACS omega. 2025; 10(8):7549-7582. DOI: https://doi.org/10.1021/acsomega.4c11045
27. Shahzadi S, Fatima S, Shafiq Z, Janjua MRSA. A review on green synthesis of silver nanoparticles (SNPs) using plant extracts: a multifaceted approach in photocatalysis, environmental remediation, and biomedicine. RSC Adv. 2025; 15(5):3858-3903. DOI: https://doi.org/10.1039/D4RA07519F
28. Dhir R, Chauhan S, Subham P, Kumar S, Sharma P, Shidiki A, Kumar G. Plant-mediated synthesis of silver nanoparticles: unlocking their pharmacological potential–a comprehensive review. Front bioeng biotechnol. 2024; 11:1324805. DOI: https://doi.org/10.3389/fbioe.2023.1324805
29. Kar AK, Singh A, Singh D, Shraogi N, Verma R, Saji J, Jagdale P, Ghosh D, Patnaik S. Biopolymeric composite hydrogel loaded with silver NPs and epigallocatechin gallate (EGCG) effectively manages ROS for rapid wound healing in type II diabetic wounds. Int J Biol Macromol. 2022; 218:506-518. DOI: https://doi.org/10.1016/j.ijbiomac.2022.06.196
30. Ahmad A, Haneef M, Ahmad N, Kamal A, Jaswani S, Khan F. Biological synthesis of silver nanoparticles and their medical applications. World Acad Sci J. 2024; 6(3):22. DOI: https://doi.org/10.3892/wasj.2024.237
31. Yi Q, Huang Z, Tang B. Impact of Silver Dressings on Wound Healing Rate in Patients with Lower Extremity Ulcers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Med Princ Pract. 2025; 34(1):13-24. DOI: https://doi.org/10.1159/000541331
32. Jain K, Takuli A, Gupta TK, Gupta D. Rethinking nanoparticle synthesis: a sustainable approach vs. traditional methods. Chem Asian J. 2024; 19(21):e202400701. DOI: https://doi.org/10.1002/asia.202400701
33. Aryani R, Nugroho RA, Manurung H, Rulimada MH, Maytari E, Siahaan A, Rudianto R, Jati WN. Anti-angiogenic activity of Ficus deltoidea L. Jack silver nanoparticles using chorioallantoic membrane assay. F1000Res. 2023; 12(1):544-560. DOI: https://doi.org/10.12688/f1000research.130477.1
34. Antunes Filho S, Almeida CM, Romanos MTV, Pizzorno Backx B, Regina Bonelli R. Green synthesis of silver nanoparticles for functional cotton fabrics: antimicrobial efficacy against multidrug-resistant bacteria and cytotoxicity evaluation. Artif Cells Nanomed Biotechnol. 2025; 53(1):153-165. DOI: https://doi.org/10.1080/21691401.2025.2485115
35. Das R, Kumar P, Singh AK, Agrawal S, Albukhaty S, Bhattacharya I, Tiwari KN, Mishra SK, Tripathi AK, AlMalki FA. Green synthesis of silver nanoparticles using Trema orientalis (L.) extract and evaluation of their antibacterial activity. Green Chem Lett Rev. 2025; 18(1):1-14. DOI: https://doi.org/10.1080/17518253.2024.2444679
36. Karimi M, Parsaei P, Asadi SY, Ezzati S, Boroujeni RK, Zamiri A, Rafieian-Kopaei M. Effects of Camellia sinensis ethanolic extract on histometric and histopathological healing process of burn wound in rat. 2013; 13(1):14-19.
37. Hada A-M, Suarasan S, Muntean M, Potara M, Astilean S. Aptamer-conjugated gold nanoparticles for portable, ultrasensitive naked-eye detection of C-reactive protein based on the Tyndall effect. Anal Chim Acta. 2024; 1307:342626-342637. DOI: https://doi.org/10.1016/j.aca.2024.342626
38. Yuan K, Sun Y, Liang F, Pan F, Hu M, Hua F, Yuan Y, Nie J, Zhang Y. Tyndall-effect-based colorimetric assay with colloidal silver nanoparticles for quantitative point-of-care detection of creatinine using a laser pointer pen and a smartphone. RSC Adv. 2022; 12(36):23379-23386. DOI: https://doi.org/10.1039/D2RA03598G
39. Barzinjy AA, Haji BS. Green synthesis and characterization of Ag nanoparticles using fresh and dry Portulaca oleracea leaf extracts: Enhancing light reflectivity properties of ITO glass. Micro nano lett. 2024; 19(3):1-13. DOI: https://doi.org/10.1049/mna2.12198
40. Ezeh CK, Eze CN, Dibua MUE, Emencheta SC. A review on Azadirachta indica (neem) plant mediated biosynthesis, characterisation and antimicrobial activity of silver nanoparticles. IJBNN. 2024; 5(1):15-36. DOI: https://doi.org/10.1504/IJBNN.2024.139351
41. Moodley JS, Krishna SBN, Pillay K, Sershen f, Govender P. Green synthesis of silver nanoparticles from Moringa oleifera leaf extracts and its antimicrobial potential. Adv Nat Sci Nanosci Nanotechnol. 2018; 9(1):015011. DOI: https://doi.org/10.1088/2043-6254/aaabb2
42. Bunawan H, Amin NM, Bunawan SN, Baharum SN, Mohd Noor N. Ficus deltoidea Jack: a review on its phytochemical and pharmacological importance. Evid Based Complement Alternat Med. 2014; 2014(1):902734. DOI: https://doi.org/10.1155/2014/902734
43. Habeeb Rahuman HB, Dhandapani R, Narayanan S, Palanivel V, Paramasivam R, Subbarayalu R, Thangavelu S, Muthupandian S. Medicinal plants mediated the green synthesis of silver nanoparticles and their biomedical applications. IET nanobiotechnol. 2022; 16(4):115-144. DOI: https://doi.org/10.1049/nbt2.12078
44. Kirubakaran D, Wahid JBA, Karmegam N, Jeevika R, Sellapillai L, Rajkumar M, SenthilKumar KJ. A Comprehensive Review on the Green Synthesis of Nanoparticles: Advancements in Biomedical and Environmental Applications. Biomed Mater Devices. 2025; 1(1):1-13. DOI: https://doi.org/10.1007/s44174-025-00295-4
45. Chandrasekaran M, Chinnaiyan U, Sivaprakasam S. Biogenic Synthesis and Characterization of Silver Nanoparticles Using a Combined Leaf Extract for Anti-Bacterial and Biofilm Inhibition Properties. Trop J Pharm Res. 2025; 9(3):1089-1096. DOI: https://doi.org/10.26538/tjnpr/v9i3.25
46. Vanlalveni C, Lallianrawna S, Biswas A, Selvaraj M, Changmai B, Rokhum SL. Correction: green synthesis of silver nanoparticles using plant extracts and their antimicrobial activities: a review of recent literature. RSC Adv. 2022; 12(25):16093-16093. DOI: https://doi.org/10.1039/D2RA90055F
47. Kantoma D, Nwokem CO. Green Synthesis of Silver Nanoparticles (AgNPs) using Calotropis procera Leaves Extract and it Adsorption Properties for the Removal of Cr3+ from Petroleum Waste Water. Comm Phy Sci. 2023; 10(3):214-223.
48. Abdel-Rahman LH, Al-Farhan BS, Abou El-ezz D, Abd–El Sayed MA, Zikry MM, Abu-Dief AM. Green Biogenic Synthesis of Silver Nanoparticles Using Aqueous Extract of Moringa oleifera: Access to a Powerful Antimicrobial, Anticancer, Pesticidal and Catalytic Agents. J Inorg Organomet Polym Mater. 2022; 32(4):1422-1435. DOI: https://doi.org/10.1007/s10904-021-02186-9
49. Kaur R, Avti P, Kumar V, Kumar R. Effect of various synthesis parameters on the stability of size controlled green synthesis of silver nanoparticles. Nano Express. 2021; 2(2):020005-020019. DOI: https://doi.org/10.1088/2632-959X/abf42a
50. Alam A, Mazumder PM. The Application of Ficus Species in the Treatment of Neurological Disorders. Pharmacogn Mag. 2024; 21(2):323–335. DOI: https://doi.org/10.1177/09731296241281440
51. Gunti H, Gaddam SA, Nadipi R, Kotakadi VS. Optical and Paper-based Dual Sensing of Hg2+ and Colorimetric Reduction of Cr (VI) by Green Synthesized Silver Nanoparticles Prepared from the Bark Extract of Sweetinia mahagoni and Their Promising Antimicrobial Applications. Nano Biomed Eng. 2023; 15(1):60-73. DOI: https://doi.org/10.26599/NBE.2023.9290012
52. Nagaraja SK, Niazi SK, Bepari A, Assiri RA, Nayaka S. Leonotis nepetifolia flower bud extract mediated green synthesis of silver nanoparticles, their characterization, and in vitro evaluation of biological applications. Materials. 2022; 15(24):8990-9010. DOI: https://doi.org/10.3390/ma15248990
53. Dubey N, Dubey N. Current regulatory framework in nanotechnology and medicine. Nanotechnology in Medicine: Toxicity and Safety. 2021:373-406. DOI: https://doi.org/10.1002/9781119769897.ch17
54. Labuda J, Barek J, Gajdosechova Z, Goenaga-Infante H, Johnston LJ, Mester Z, Shtykov S. Analytical chemistry of engineered nanomaterials: Part 1. Scope, regulation, legislation, and metrology (IUPAC Technical Report). PAC. 2023; 95(2):133-163. DOI: https://doi.org/10.1515/pac-2021-1001
55. Din SM, Malek NANN, Shamsuddin M, Matmin J, Hadi AA, Asraf MH. Antibacterial silver nanoparticles using different organs of Ficus deltoidea Jack var. kunstleri (King) Corner. Biocatal Agric Biotechno. 2022; 44:102473. DOI: https://doi.org/10.1016/j.bcab.2022.102473
56. Ismail IQ, Malek NANN, Sani NS, Din SM, Asraf MH. Green Biosynthesized Silver Nanoparticles using Ficus deltoidea Leaf Extract as Antibacterial Agent. Bioresour Enviro. 2023; 1(3):27-44. DOI: https://doi.org/10.24191/bioenv.v1i3.34
57. Sharma K, Guleria S, Razdan VK. Green synthesis of silver nanoparticles using Ocimum gratissimum leaf extract: characterization, antimicrobial activity and toxicity analysis. J Plant Biochem Biotechnol. 2020; 29(2):213-224. DOI: https://doi.org/10.1007/s13562-019-00522-2
58. Mamouni R, Jadouali S, Atifi H, Saffaj N, Chartier A, Nehme R, Boussif K, Achemchem F. A novel green reducing agent for the synthesis of chromium oxide nanoparticles (Cr2O3 NPs) based on saffron by-products: Characterization and antioxidant activity. Mater Sci Eng B. 2024; 305:117415. DOI: https://doi.org/10.1016/j.mseb.2024.117415
59. Terenteva E, Apyari V, Dmitrienko S, Zolotov YA. Formation of plasmonic silver nanoparticles by flavonoid reduction: A comparative study and application for determination of these substances. SAA. 2015; 151:89-95. DOI: https://doi.org/10.1016/j.saa.2015.06.049
60. Godeto YG, Ayele A, Ahmed IN, Husen A, Bachheti RK. Medicinal plant-based metabolites in nanoparticles synthesis and their cutting-edge applications: an overview. 2023; 1(1):1-34. DOI: https://doi.org/10.1201/9781003213727-1
61. Khan MR, Ahmad K, Akram R, Asif HM, Ahmad B, Ali T, Anjum I, Sami A, Bibi A, Saifullah S. Green synthesis, characterization and antibacterial potential of silver nanoparticles from Onosma bracteatum extract. Trop J Pharm Res. 2022; 6(2):202-206.
62. Alharbi NS, Alsubhi NS. Silver Nanoparticles Biosynthesized Using Azadirachta indica Fruit and Leaf Extracts: Optimization, Characterization, and Anticancer Activity. J Nanomater. 2023; 2023(1):1-17. DOI: https://doi.org/10.1155/2023/9916777
63. Lan-Chi NT, Narayanan M, Chinnathambi A, Govindasamy C, Subramani B, Brindhadevi K, Pimpimon T, Pikulkaew S. Fabrication, characterization, anti-inflammatory, and anti-diabetic activity of silver nanoparticles synthesized from Azadirachta indica kernel aqueous extract. Environ Res. 2022; 208:112684. DOI: https://doi.org/10.1016/j.envres.2022.112684
64. Liu L, Yu C, Ahmad S, Ri C, Tang J. Preferential role of distinct phytochemicals in biosynthesis and antibacterial activity of silver nanoparticles. J Environ Manage. 2023; 344:118546. DOI: https://doi.org/10.1016/j.jenvman.2023.118546
65. Reddy K, Salve P. Biogenic synthesis of silver nanoparticles from Hylocereus undatus peel waste: exploring EGFR inhibition for targeted therapy of cervical and breast carcinomas. Futur J Pharm Sci. 2024; 10(1):160. DOI: https://doi.org/10.1186/s43094-024-00737-8
66. Elish SEAA, Temraz A, Hassan Baky M. Phytochemical diversity of genus Ficus: A mini review. ERU Res J. 2023; 2(3):502-524. DOI: https://doi.org/10.21608/erurj.2023.310215
67. Ikhsan AN, Syifa F, Mustafidah M, Rohman A. Implementation of chemometrics as a Solution to detecting and preventing falsification of herbal medicines in Southeast Asia: A review. J Appl Pharm Sci. 2021; 11(9):139-148.
68. Samsulrizal N, Yong-Meng G, Ahmad H, Syimal’ain Azmi N, Mohamad Zin NSN, Mahdi E. Infrared spectral markers for the nephroprotective effects of Ficus deltoidea in streptozotocin-induced diabetic rats. BioRxiv. 2020; 1(1):1-37. DOI: https://doi.org/10.1101/2020.12.23.424120
69. Sidhu AK, Verma N, Kaushal P. Role of biogenic capping agents in the synthesis of metallic nanoparticles and evaluation of their therapeutic potential. Front Nanotechnol. 2022; 3:801620-801637. DOI: https://doi.org/10.3389/fnano.2021.801620
70. Zhu W, Wu J, Guo X, Sun X, Li Q, Wang J, Chen L. Development and physicochemical characterization of chitosan hydrochloride/sulfobutyl ether-β-cyclodextrin nanoparticles for cinnamaldehyde entrapment. J Food Biochem. 2020; 44(6):e13197. DOI: https://doi.org/10.1111/jfbc.13197
71. Agressott EVH, Blätte D, Cunha FA, Noronha VT, Ciesielski R, Hartschuh A, Paula AJ, Fechine PBA, Souza Filho AG, Paschoal AR. Vibrational Spectroscopy and Morphological Studies on Protein-Capped Biosynthesized Silver Nanoparticles. ACS omega. 2020; 5(1):386-393. DOI: https://doi.org/10.1021/acsomega.9b02867
72. Santhanam R, Sivapragasam G, Karunakaran T, Muniandy K, Kandasamy SP, Palanisamy A. Identification of chemical constituents and inhibitory effect of Ficus deltoidea fraction against lipopolysaccharide-induced nuclear factor-kappa B inflammatory pathway in murine macrophage 264.7 cells. harmacogn Mag. 2021; 17(74):236-243. DOI: https://doi.org/10.4103/pm.pm_433_20
73. Renuka R, Thilagavathi T, Inmozhi C, Uthrakumar R, Rajasaravanan ME, Kaviyarasu K, Al-Taisan NA, Awad M, Alam MW. Phytochemical Investigation and Characterization of Azadirachta Indica-Mediated Silver Nanoparticles and Their Potential as Antibacterial and Antidiabetic Agents. 2024; 19(10):2450061. DOI: https://doi.org/10.1142/S1793292024500619
74. Sulaiman M, Muhammad MaA, Sulaiman AS, Abubakar AL, Sharma R, Shuaibu AM, Aliyu M, Mustapha ITu, Tiwari R. Antimicrobial Potential and Characterization of Silver Nanoparticles Synthesized from Ocimum sanctum Extract. 2024; 1(1):1-16. DOI: https://doi.org/10.1101/2024.09.19.613829
75. Bold BE, Urnukhsaikhan E, Mishig-Ochir T. Biosynthesis of silver nanoparticles with antibacterial, antioxidant, anti-inflammatory properties and their burn wound healing efficacy. Front chem. 2022; 10:972534. DOI: https://doi.org/10.3389/fchem.2022.972534
76. Islam A, Mandal C, Habib A. Antibacterial potential of synthesized silver nanoparticles from leaf extract of Moringa oleifera. J Adv Biotechnol Exp Ther. 2021 2021; 4(1):67. DOI: https://doi.org/10.5455/jabet.2021.d108
77. Mehwish HM, Liu G, Rajoka MSR, Cai H, Zhong J, Song X, Xia L, Wang M, Aadil RM, Inam-Ur-Raheem M, Xiong Y, Wu H, Amirzada MI, Zhu Q, He Z. Therapeutic potential of Moringa oleifera seed polysaccharide embedded silver nanoparticles in wound healing. Int J Biol Macromol. 2021; 184:144-158.
78. Adeyemi OS, Shittu EO, Akpor OB, Rotimi D, Batiha GE-s. Silver nanoparticles restrict microbial growth by promoting oxidative stress and DNA damage. EXCLI J. 2020; 19:492.
79. Rodrigues AS, Batista JG, Rodrigues MÁ, Thipe VC, Minarini LA, Lopes PS, Lugão AB. Advances in silver nanoparticles: a comprehensive review on their potential as antimicrobial agents and their mechanisms of action elucidated by proteomics. Front Microbiol. 2024; 15:1440065. DOI: https://doi.org/10.3389/fmicb.2024.1440065
80. Aguilera Stewart C, Alar C, Bargsted L, Kaklamanou I, Gozza GA, Polito MP, Enzo E, Sifrim A, Aragona M. Defining the role of fibroblasts in skin expansion. BioRxiv. 2025; 1(1):2025-2078. DOI: https://doi.org/10.1101/2025.03.18.643853
81. Dong X, Xiang H, Li J, Hao A, Wang H, Gou Y, Li A, Rahaman S, Qiu Y, Li J, Mei O, Zhong J, You W, Shen G, Wu X, Li J, Shu Y, Shi LL, Zhu Y, Reid RR, He TC, Fan J. Dermal fibroblast-derived extracellular matrix (ECM) synergizes with keratinocytes in promoting re-epithelization and scarless healing of skin wounds: Towards optimized skin tissue engineering. Bioact Mater. 2025; 47(1):1-17. DOI: https://doi.org/10.1016/j.bioactmat.2024.12.030
82. Jacob JA, Mahal HS, Biswas N, Mukherjee T, Kapoor S. Role of phenol derivatives in the formation of silver nanoparticles. Langmuir. 2008; 24(2):528-533. DOI: https://doi.org/10.1021/la702073r
83. Moond M, Singh S, Sangwan S, Devi R, Beniwal R. Green Synthesis and Applications of Silver Nanoparticles: A Systematic Review. AATCC J Res. 2022; 9(6):272-285. DOI: https://doi.org/10.1177/24723444221119847
84. Sarika Ankushrao N, Shilpa Pravin C. Biosynthesis of Silver Nanoparticles from Polyphenolic Extract of Baliospermun solanifolium using Central Composite Design. Pharmacog Res. 2022; 14(4):405-411. DOI: https://doi.org/10.5530/pres.14.4.59
85. Liu H, Chen L, Peng Y, Li X, Zhang H, Chen Y, Li Z, Dai F. A tea polyphenol-loaded cellulose/silk fibroin/polyacrylic acid hydrogel for wound healing. Cellulose. 2024; 31(13):8169-8187. DOI: https://doi.org/10.1007/s10570-024-06102-5
86. Tong MQ, Lu CT, Huang LT, Yang JJ, Yang ST, Chen HB, Xue PP, Luo LZ, Yao Q, Xu HL, Zhao YZ. Polyphenol-driven facile assembly of a nanosized acid fibroblast growth factor-containing coacervate accelerates the healing of diabetic wounds. Acta Biomater. 2023; 157:467-486. DOI: https://doi.org/10.1016/j.actbio.2022.11.054
87. Mehwish HM, Liu G, Rajoka MSR, Cai H, Zhong J, Song X, Xia L, Wang M, Aadil RM, Inam-Ur-Raheem M. Therapeutic potential of Moringa oleifera seed polysaccharide embedded silver nanoparticles in wound healing. Int J Biol Macromol. 2021; 184:144-158. DOI: https://doi.org/10.1016/j.ijbiomac.2021.05.202
88. Galdopórpora JM, Ibar A, Tuttolomondo MV, Desimone MF. Dual-effect core–shell polyphenol coated silver nanoparticles for tissue engineering. Nano-Struct Nano-Objects. 2021; 26:100716. DOI: https://doi.org/10.1016/j.nanoso.2021.100716